TUESDAY, July 21, 2015 (HealthDay News) — The antibiotic dicloxacillin may lessen the effects of some blood-thinning medications, new research shows.
“The surprise in the study was just how much of an impact dicloxacillin had,” said study author Anton Pottegard, a pharmacist and research fellow at the University of Southern Denmark, in Odense.
“Often, the effects in these kinds of studies are quite small. But this was very pronounced: Six out of 10 patients dropped so much in their level of blood-thinning that they were no longer sufficiently protected against clotting and stroke,” Pottegard said.
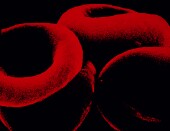
Coumadin (warfarin) and similar blood thinners lower the risk of blood clots, a potential cause of strokes and heart attacks, by thinning the blood so blockages don’t form in vessels, according to the U.S. National Library of Medicine. Patients with irregular heart rhythms, such as atrial fibrillation, and those who’ve had heart valves replaced often take these medications.
Physicians order blood tests for patients while they’re on the medication, to make sure the dose they’re taking is causing the proper level of blood-thinning.
“When its levels are too high, patients are at risk for life-threatening bleeding events. When too low, patients may be at risk for blood clots, stroke or pulmonary [clots],” said Dr. Mike Lane, an assistant professor of medicine in the infectious diseases division at the Washington University School of Medicine in St. Louis.
Physicians also know that a wide variety of drugs, including some antibiotics, can disrupt the effects of Coumadin.
“Unfortunately, it has many drug interactions that makes it challenging to use. Some medications may increase the effect while others decrease the effect. Unfortunately, we only know about some of these interactions through small case reports,” Lane said.
In the new study, researchers pinpointed an apparent interaction between Coumadin and dicloxacillin, a medication used to treat infections that don’t respond to penicillin.
“Although dicloxacillin is not used frequently in the United States, similar antibiotics are commonly used,” Lane noted.
In the new study, researchers looked at almost 250 people who took Coumadin and dicloxacillin. Their average age was 68, and 61 percent were male. The researchers found that blood thinning in 61 percent of the patients became less effective within two to four weeks after treatment with the antibiotic.
The reasons for the interaction aren’t clear. But, Pottegard said it appears that the antibiotic affects how the liver processes the blood thinner, which may cause faster elimination of the blood thinner from the body.
Pottegard says physicians should be cautious about prescribing dicloxacillin in patients who take Coumadin or similar blood thinners.
If the antibiotic is absolutely necessary, he said, doctors should closely monitor the level of blood thinning during treatment and for one to two weeks after patients stop taking the antibiotic.
As for the new generation of blood thinners that work in a different way than Coumadin — including Eliquis, Xarelto and Pradaxa — Pottegard said there’s no reason to think the antibiotic would have the same effect with them.
The study appears in the July 21 issue of the Journal of the American Medical Association.
More information
For more about blood thinners, try the U.S. Agency for Healthcare Research and Quality.
Copyright © 2026 HealthDay. All rights reserved.

