FRIDAY, May 1, 2020 (HealthDay News) — Many people who are seriously ill with COVID-19 end up on ventilators to help them breathe, but sometimes, even ventilators aren’t enough. That’s when a device called ECMO may help.
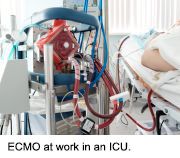
ECMO can do the work of the lungs and in some cases, the heart. ECMO stands for extracorporeal membrane oxygenation. It’s a machine that oxygenates blood using a complex circuit of pumps, tubes, filters and monitors. Someone on ECMO has to be monitored by a team of experts, and it’s not available in all hospitals.
“ECMO doesn’t do anything to treat COVID-19, but it buys you time by replacing the function of the lungs to allow recovery of the lungs,” explained Dr. Jonathan Haft, director of the ECMO program at the University of Michigan in Ann Arbor.
Dr. John Puskas, chair of cardiovascular surgery at Mount Sinai Morningside in New York City, said ECMO is typically used when “patients get to a point where the ventilator is not enough.”
He said that ECMO has a “fancy membrane that can exchange gases. It gets rid of carbon dioxide and adds oxygen to the blood, basically replacing the lungs. ECMO is remarkably effective at adding oxygen to the blood.” And oxygen is just what many COVID-19 patients desperately need.
Currently, the Extracorporeal Life Support Organization (ELSO) reports that more than 400 people are on ECMO for COVID-19 in North America. Haft said membership in ELSO is voluntary and he believes the database may only represent about half of the ECMO use in the United States.
One drawback, however, is that ECMO isn’t nearly as available as ventilators are. It’s also far more labor-intensive to manage than ventilators.
Still, the World Health Organization has suggested that medical centers capable of providing ECMO should consider it in COVID-19 patients with very low oxygen levels despite other treatments, according to a viewpoint published recently in the Journal of the American Medical Association.
But the viewpoint authors pointed out that “ECMO is not a therapy to be rushed to the frontline when all resources are stretched in a pandemic.”
Puskas agreed. “I don’t think ECMO is a panacea for COVID. In a large majority of COVID patients, it should not be used.”
Because the pandemic is so new, there isn’t yet a lot of information on what the benefits and risks might be when using ECMO in COVID-19 patients, or which patients might fare best with ECMO.
“We’ve been struggling with patient selection. Patients may not tolerate ECMO if they have some of the inflammation linked to COVID or the multisystem organ failure seen with COVID. We want to give ECMO to patients who can benefit from it,” Puskas explained.
Haft agreed that patient selection has been difficult. “There is a finite capacity, so you have to be thoughtful about who receives ECMO in the context of a pandemic. When patients go on ECMO, it takes a long time for them to recover to the point where they can leave the hospital.” He added that the average time on ECMO for COVID-19 patients is nine days.
Major factors in choosing who might go on ECMO include things that influence survival odds, such as age, other health conditions and overall health and function prior to the illness, Haft said.
He noted the biggest risks associated with ECMO are excess bleeding or clotting, and infection.
Dr. Gabriele Di Luozzo, who directs thoracic aortic surgery at Mount Sinai Morningside, said with COVID-19 patients, “Clotting has been a big concern. We have to keep their blood thin with medications, but it’s been a challenge to figure out how thin we need to maintain their blood.”
Haft said that “ECMO can be effective for selected patients with COVID, but ECMO requires a team and it has to be performed at a center that has experience.”
More information
Learn more about ECMO from the University of California, San Francisco.
Copyright © 2026 HealthDay. All rights reserved.