THURSDAY, Oct. 31 (HealthDay News) — Many people living with Parkinson’s disease suffer from hallucinations and delusions, but an experimental drug might offer some relief without debilitating side effects.
The drug — pimavanserin — appears to significantly relieve these troubling symptoms, according to the results of a phase 3 trial to test its effectiveness.
Such symptoms affect as many as half of the estimated 7 million to 10 million Parkinson’s patients around the world, according to study background information.
Currently, patients are treated with antipsychotic drugs such as clozapine and quetiapine, which worsen Parkinson’s motor symptoms, hasten mental decline, increase the risk of stroke and can be life-threatening, authors of the new study said.
Their study was published in the Nov. 1 online issue of The Lancet and funded by Acadia Pharmaceuticals, the makers of pimavanserin.
“There are no first-line approved treatments for psychosis in people with Parkinson’s disease,” said lead researcher Dr. Clive Ballard, a professor of age-related diseases at King’s College, London.
“Existing antipsychotics are either ineffective or not tolerated. Pimavanserin is not yet licensed, but could potentially offer a change in the treatment of these distressing and impactful symptoms,” he said.
An expert not involved with the study talked about the need for a medication alternative.
“The Parkinson’s disease community has been waiting for a potentially new approach for the treatment of psychosis and hallucinations,” said Dr. Michael Okun, national medical director of the National Parkinson Foundation.
“Pimavanserin may offer a relatively safe and reasonably efficacious choice for many patients in the situation where the current therapies are not adequate,” Okun added.
The new drug works differently from other antipsychotics, study author Ballard said.
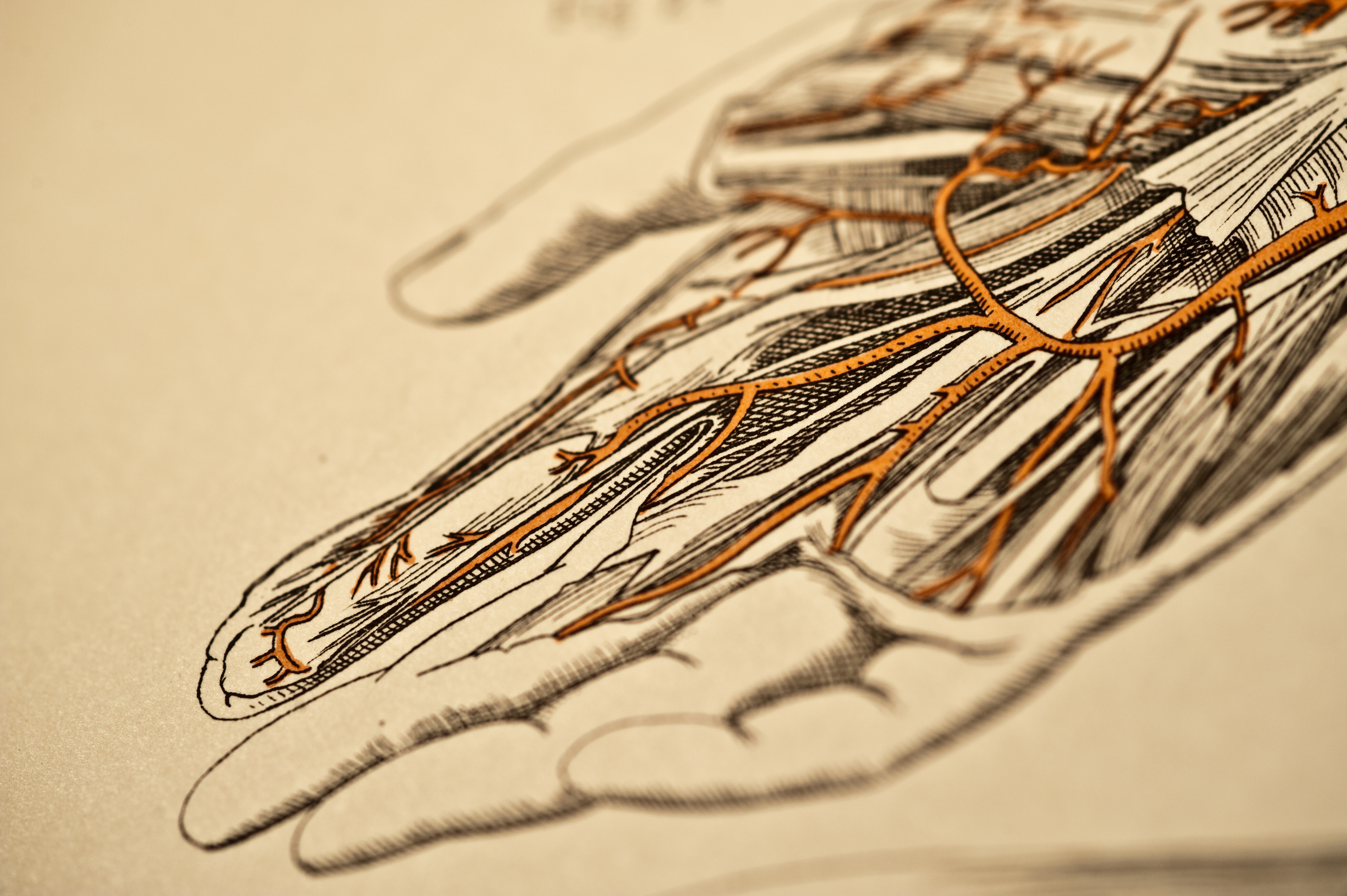
Pimavanserin blocks certain receptors — called serotonin 5-HT2A receptors — in the neocortex of the brain. This part of the brain is responsible for sensory perceptions, conscious thought and language, and is associated with hallucinations and delusions, Ballard explained.
For the trial, Ballard’s team randomly assigned 199 Parkinson’s patients suffering from disease-associated psychosis to daily doses either of pimavanserin or an inactive placebo pill.
After 43 days, patients taking pimavanserin showed a significant improvement on a scale of psychotic symptoms compared to those given a placebo — 37 percent versus 14 percent.
However, this early study only provided short-term results, another expert pointed out.
Frances Weaver, director of the Center for Management of Complex Chronic Care at Hines VA Hospital, in Illinois, said although the trial was promising, more needs to be known about the long-term picture for this drug.
“The follow-up was only 43 days,” she said. “It will be important to examine the long-term effects of this medication as psychosis is an ongoing problem which will likely require the patient to remain on medications for the rest of his life. Questions about long-term tolerability and effectiveness still need to be answered.”
In addition to psychosis relief, the researchers reported other benefits of the drug. Patients taking pimavanserin slept better and the improvement in mental functioning also helped caregivers, who found it easier to care of their patients, Ballard said.
Motor symptoms of the people taking the drug didn’t get worse, the study found.
Dr. Susan Fox, an associate professor of neurology at the University of Toronto, wrote an accompanying journal editorial about the new findings.
“Treating psychosis in Parkinson’s disease is challenging because of side effects of current drugs — especially potentially worsening Parkinson’s disease motor symptoms. Pimavanserin offers an alternative without this risk,” Fox said.
Pimavanserin was well tolerated and side effects were mild to moderate, and similar in the two groups. The most common side effects were urinary tract infections (12 percent for placebo versus 13 percent for pimavanserin) and falls (9 percent for placebo versus 11 percent for pimavanserin), the researchers found.
However, 10 patients stopped taking pimavanserin because of a side effect, compared with two patients in the placebo group, the authors noted.
According to Ballard, the U.S. Food and Drug Administration has invited a new drug application based on this trial, “so the decision regarding approval should probably be in 12 to 18 months,” he said.
More information
To find out more about Parkinson’s disease, visit the U.S. National Institute of Neurological Disorders and Stroke.
Copyright © 2025 HealthDay. All rights reserved.