WEDNESDAY, Sept. 25 (HealthDay News) — Kidney transplant patients who develop a specific type of antibody response may be at particular risk of having the organ fail within a few years, a new study suggests.
Experts said the results could help pinpoint those who are at the highest risk of a transplant failure — and possibly aid in finding a good donor organ for some patients.
“This is a very exciting paper,” Dr. Jacqueline Lappin, a transplant surgeon at Scott & White Healthcare in Temple, Texas, said of the study, which appears in the Sept. 26 issue of the New England Journal of Medicine.
Lappin, who was not involved in the research, said the findings give insight into the specific type of immune response that is dangerous to a donor organ. And that could have implications for patients both before and after a kidney transplant, she added.
For the study, French researchers followed 1,016 patients who received donor kidneys at two Paris transplant centers. They wanted to see whether patients who developed a particular type of antibody against the donor organ would be at increased risk of having the transplant fail in the next few years.
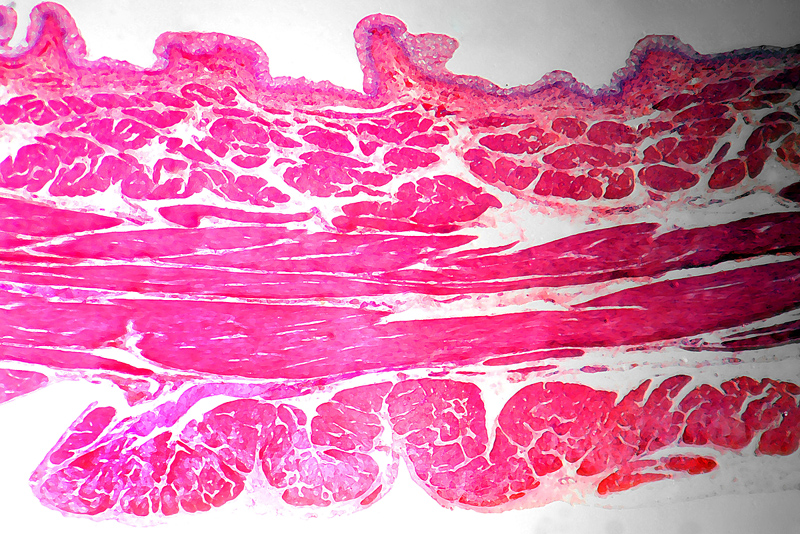
The research focused on so-called anti-HLA antibodies. HLAs are proteins on the surface of white blood cells and other tissues; if a kidney donor’s HLAs do not fully match a recipient’s, the recipient’s immune system will develop anti-HLA antibodies.
But while those antibodies may attack and severely injure the donor kidney in some patients, they may do little to no damage in others — suggesting not all anti-HLA antibodies are bad news.
“What we’ve been grappling with is, what is a ‘relevant’ antibody?” Lappin said.
Based on the new findings, the anti-HLA antibodies that are a problem can be distinguished by whether they bind to an immune system protein called C1q. The 77 patients with C1q-binding antibodies were at much higher risk of having the donor kidney fail, according to the researchers.
Only 54 percent of those patients saw their kidney “survive” for five years, vs. about 94 percent of patients with either no anti-HLA antibodies or anti-HLA antibodies that did not bind to C1q.
An antibody’s ability to bind to C1q is key because it activates a part of the immune system called the complement system, which helps antibodies fight foreign invaders.
The new findings suggest that measuring the “complement-binding” capacity of anti-HLA antibodies could help spot patients at particular risk of a donor kidney loss, according to the research team, led by Dr. Alexandre Loupy of the French national research institute INSERM.
The results are “intriguing” and “certainly advance the field,” said Dr. Lorraine Racusen, a pathology professor at Johns Hopkins University in Baltimore.
But there are still questions to answer before such testing comes into routine use, according to Racusen, who wrote an editorial published with the study.
A big one is whether C1q antibodies respond to therapy, and whether that will actually improve how patients fare, she said. There are potential ways to lower patients’ antibody levels: One, Racusen said, is to filter them from the blood in a process called plasmapheresis; another is treatment with medications like intravenous immunoglobulin.
Racusen said that measuring this particular characteristic of patients’ anti-HLA antibodies “adds some refinement” to gauging the risk of kidney loss. But, she added, “is this something that people need to implement now? No, I don’t think so.”
Lappin said she thinks the “most exciting” potential use could be in the period where doctors are trying to find a good donor-recipient match — particularly for “sensitized” patients.
About 30 percent of people who need a donor kidney are considered sensitized, which means they have a high level of anti-HLA antibodies. They have those antibodies as a result of past exposure to foreign tissue — either from a previous kidney transplant, or from another source, like a blood transfusion or pregnancy.
It’s estimated that sensitized patients wait three to four times longer for a compatible kidney from a deceased donor, vs. non-sensitized patients.
When a potential donor kidney is found, doctors perform a “cross-match” test, which involves mixing a blood sample from the recipient with blood cells from the donor. If the result is “positive,” that means the patient has anti-HLA antibodies against that donor’s tissue.
In those cases, patients may be able to have the anti-HLA antibodies removed, in what doctors call “desensitization.” Even after that process, though, the donor organ can still be rejected, and the cost of desensitization ranges from $20,000 to $30,000 — which may or may not be covered by insurance.
But Lappin said the new results present the possibility that if patients’ antibodies are not of the C1q-binding variety, the donor kidney could still be suitable.
“That could potentially give sensitized patients more options,” she said.
In the United States, almost 98,000 people are currently on the waiting list to get a donor kidney, according to the Organ Procurement and Transplantation Network.
More information
The U.S. National Institute of Diabetes and Digestive and Kidney Diseases has more on kidney transplants.
Copyright © 2026 HealthDay. All rights reserved.